GENERAL MEDICINE CASE DISCUSSION of 17 year old female
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians signed informed consent.
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Case Scenario:
A 17 year old female student by occupation presented to causality on 1/5/2021 with
Chief complaints of
1.Involuntary movements of both upper and lower limbs a day before.
History of present illness:
Patient was apparently asymptomatic one day ago, then she developed recurrent involuntary movements of all four limbs associated with loss of consciousness and frothing. And with recovery of consciousness in between episodes with post ictal confusion lasting for 30 secs to few minutes.
No. of episodes are 5 to 6 in 24 hours.
she first visited hospital 1 And was then referred to hospital 2 for further management.
She continued to have multiple GTCS episodes with a frequency of one in 20 minutes.
She also complained of
*Headache which was right sided,intermittent ,dull aching type.
*vomitings:1 episode of vomiting bilious,containing food particles.
*No h/o involuntary micturition,No h/o involuntary defecation
*No H/o tongue bite.
*No H/o fever,cough,SOB,chestpain,sweating.
*No H/o weakness of limbs.
,PAST HISTORY:
No H/o similar complaints in the past
Not a known case of Hypertension ,TB,Bronchial Asthma,thyroid, CAD.
TREATMENT HISTORY
Not on any medication
SURGICAL HISTORY:
NO H/O any surgeries in the past
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep:Adequate
Bowel and bladder movements: Regular
Allergies:No
Addictions:No
FAMILY HISTORY:
No H/o Similar complaints in the family.
Her father is a known case of hypertension since 2years.
MENSTRUAL HISTORY:
Age of menarche: 13 years
Menstrual cycle: Regular
PHYSICAL EXAMINATION:
Patient is conscious coherent and cooperative
Moderately built and moderately nourished
Well oriented to time place and person
VITALS
TEMPERATURE: Febrile
Pulse rate: 89bpm
BP: 110/80 mmhg
Spo2:99%. At room air
Pallor present
No icterus
No cyanosis
No clubbing
No lymphadenopathy
No edema
SYSTEMIC EXAMINATION:
CNS EXAMINATION
She is conscious coherent and coperative
Speech: Normal
No neck stiffness
Kerning sign: negative
Power and tone :Normal
Reflexes:
Biceps: Right +++ Left+++
Triceps:Right +++ Left+++
Supinator:Right +++ Left+++
Knee:Right +++ Left+++
Ankle:Right + Left+
CVS EXAMINATION:
Cardiac sounds S1 S2 heard
No murmers heard
RESPIRATORY SYSTEM
Normal vesicular breath sounds heard
Trachea: central
No wheeze
ABDOMEN EXAMINATION:
Shape of abdomen: scaphoid
No tenderness
No palpable mass
Liver not palpable
INVESTIGATIONS:
MRI
HEMOGRAM
RFT
RBS
CHEST XRAY
COMPLETE URINE EXAMINATION
LIVER FUNCTION TESTS
ECG
CBP:

Impression:Microcytic hypochromic anemia with lymphocytic leucocytosis.
CUE
2/5/21
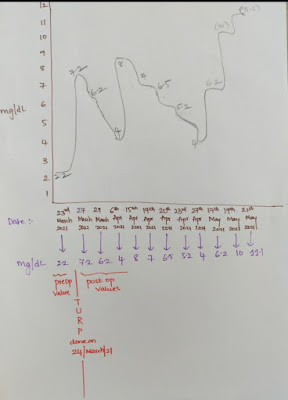
SERUM ELECTROLYTES
 |
CBP
CBP:
Impression:Microcytic hypochromic anemia with leucocytosis.
3/5/21
APTT TEST
4/5/21
RENAL FUNCTION TEST:
Decreased sodium.
LIVERFUNCTION TESTS:
*AST elevated
Total protein and albumin are less than normal.
ABG
5/5/21
SERUM ELECTROLYTES
Potassium #3.4 decreased.
ABG
6/5/21
7/5/21
ABG:LIVER FUNCTION TESTS:
AST ALT elevated
Total protein and albumin levels reduced.
LIVER FUNCTION TESTS
Total protein and albumin levels decreased.
ABG
RFT
Microcytic hypochromic anemia.
MRI on 2/5/21
IMPRESSION ON MRI:F/S/O Acute cortical vein thrombosis with hemorrhagic venous infarction involving Right posterior temporal lobe with midline shift to left by 4mm.
Diagnosis:
Recurrent seizures(seizure clusters/status epilepticus)resolved secondary to cortical vein thrombosis with hemorrhagic venous infarction in right posterior temporal lobe with (4mm midline shift).
Iron deficiency anemia.
TREATMENT:
1.Inj Levipil 1gm in 100ml NS IV STAT
Inj Levipil 500mg iv BD
2.Inj Lorazepam iv sos
3.Inj sodium valproate 800mg/iv/stat
Inj phenytoin 800mg iv/stat
4.Inj Midazolam 0.2 mg/kg/hr
Accordingly Upto 2mg/kg
5.Inj Clexane 0.4ml s/c BD
6.Inj Dexamethasone 4mg TID
7.Inj Mannitol 100ml iv/BD
8.RT Feeds 100ml water hourly
50ml milk 2nd hourly
On 2/5/21
Patient is conscious coherent cooperative.
Afebrile to touch.
Rt sided parietal area headache.
No photophobia no vomiting.
O/E:
Pupil normal Response to light.
On 3/5/21
Seizures GTCS 7 episodes and 1 episode of high grade fever on 2nd may night .
Last seizure episode on 3rd may 9: 30 am
Decreased by inj phenobarbitone 20mg/kg-800 mg iv stat
Consciousness present in inter ictal period.
O/ E :
pt is sedated responding to painful stimuli.
E3v3M5
Pupils B/l pinpoint secondary to BZD
FEBRILE 100 F
On 4/5/21
Pt was intubated last night for recurrent seizures
Last seizure episode 10:30 pm before intubation
2 episodes of high grade fever last night
Hiccups present, edema and thrombophlebitis present.
Did not pass stool since 3 days
O/E
Febrile 100 F
Pt was sedated,moving intermittently.
Pupils pinpoint non reactive to light
Gcs:E1VTM2
On 5/5/21
Seizure free period 36hrs
High grade intermittent fever
Intermittent movement present,Thrombophlebitis and edema present.
Hiccups decreased.
O/E
Patient is sedated
E1VtM2
Temp:102.7 F
On 6/5/21
High grade fever every 4 to 5 hrs
Seizures free period 2 days
Intermittent movement present,Thrombophlebitis and edema present.
Stools not passed since 4 days
0n 7/5/21
fever frequency reduced
Seizures free period 72 hours
Intermittent movement present,
Thrombophlebitis and edema present.
Stools not passed since 5 days
O/E
Pt E4VTM6
CNS No abnormality detected
Spo2 99% on CPAP mode
On 8/5/21
Extubation yesterday
High grade fever continuosly every 4hrs
O/E
Febrile to touch 100. 2F
CNS HMF intact
Power: 4/5 in all limbs
Handgrip:70% b/l
On 9/5/21
S/p extubation
High grade fever every 4hrs
O/E
Febrile to touch 100F
CNS HMF intact
Power 4 /5 in all limbs
Handgrip 80% Bilateral
On 10/5/21
Sensorium improved
Fever spikes reduced
On 11/5/21
1 episode of GTCS yesterday on 10th may
O/E CNS No abnormality detected
12/5/21 13/5/21 no fresh complaints
14/5/21
Rx oral fluids 4 to 5 lit/ day
Encourage soft diet
Inj LEVIPIL 1gm/ iv/bd
Inj sodium valproate 1 gm 100ml NS/IV/Bd
15/5/21 no fresh complaints
16/5/21 Seizure free period since 5days
No new symptoms
O/E patient conscious and afebrile
HMF Intact
NO FND
Fundus:No papilledema
Rx change from injections to tablets
Tab sodium valproate 1gm/po/BD
T.levitiracetam 1gm/po/BD
T.ACITROM 2mg/po/OD
INJ CLEXANE 4Omg /sc/BD
T.FRISIUM 5mg/PO/OD 8.00 am
Inj Mannitol 20gm /iv/OD
T.OROFER XT /po/BD
17/5/21
Seizure free period since 6days
No new symptoms
O/E patient conscious and afebrile
HMF Intact
NO FND
18/5/21
Seizure free period since 7 days
Headache yesterday night got resolved
No new symptoms
O/E patient conscious and afebrile
HMF Intact
NO FND.
19/5/21
Seizure free period since 8 days.
CNS Higher Mental Function intact.
Rx Levipil 500mg/po/TID
COURSE IN HOSPITAL
Initially Patient was given inj Lorazepam 8mg iv stat Leviteracetam 1gm iv stat,inj sodium valproate 800mg stat started on inj Midazolam 0.2mg/kg/hr and escalated upto 2mg/kg/hr,inj Clexane 0.4ml/sc was started in suspicion of CSVT,inj Mannitol 20gmTID.
Patient continued to have seizures with decreased frequency 9thday .
MRI was done on 2/5/21 with venogram which showed cortical venous thrombosis and hemorrhagic venous infarction in post temporal.
Fundoscopy showed papilloedema in the right eye. patient was given inj phenobarbitone 20 mg/kg stat 800mg in view of recurrent seizures and need for further sedation.
Patient was electively intubated on 4/5/21 and dose of Midazolam was increased till seizure free period was achieved.
Also continued on anticoagulantion and other antiepileptics.
3 days after seizure free period patient was tapered off Midazolam, phenobarbitone and extubated on 8/5/21.
And continued on same treatment.
She had one episode of GTCS again on 10/5/21 resolved spontaneously.
She was shifted back to ICU where she was monitored Tab Acitrom 2mg was started on 16/5/21 once daily and clexane tapered off.
Possible Questions
Possible questions:1. what can be the cause of her condition ?
2. what are the risk factors for cortical vein thrombosis?
3.There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
4. What drug was used in suspicion of Cvst?







































Comments