A 55 Year Old Female with Shortness of Breath, pedal Edema and Facial Puffiness.
A 55 year old female patient, a resident of Miryalaguda and farmer by occupation came to the hospital on 17/5/21 with the chief complaints of shortness of breath, pedal edema and facial puffiness.
HISTORY OF PRESENTING ILLNESS
Patient has had episodes of shortness of breath on and off for the past 20 years.
Her first episode 20 years ago lasted for 1 week and occured in the month of january that year during which time she was working in a paddy field. This first episode was relieved upon taking medication the name of which the patient is unable to recall.
For the next 8 years the patient has suffered from similar episodes of SOB every year each lasting aproximately 1 week and occurring around January (when she worked at the paddy fields) these episodes were all relieved upon taking medication.
12 years ago she had another episode of SOB. This one lasted 20 days and she had to be hospitalized. The SOB decreased upon treatment at the hospital.
For the past 12 years she has been having an yearly episodes now lasting around a month again around january. Until her latest episode the SOB was of grade II
Her latest episode of shortness of breath started 30 days ago, her SOB was insidious in onset and gradual in progression.
Initially the SOB occurred on exertion and was relieved upon rest. From 2 days ago she started having SOB even at rest (grade IV) and was not relieved with nebulizers. No history of paroxysmal nocturnal dyspnea or Orthopnea.
She used nebulizations and inhalers for her episodes of SOB which usually treated her symptoms.
This time inspite of the same treatment the SOB progressed along with pedal edema.
She is currently being treated with intermittent BiPAP.
She was diagnosed with diabetes 8 years ago when she had seeked help for her polyuria and is being treated for it ever since.
5 years ago she was treated for anemia with iron injections.
1 month back she was experiencing generalized weakness for which she was administered IV fluids (3 pints in 2 days) by a local RMP
20 days ago due to the ongoing Covid 19 pandemic she had an HRCT outside which showed signs of bronchiectasis.
She was diagnosed with Hypertension 20 days ago and is being treated for the same.
Pedal edema since 15 days upto the level ankle and pitting type.
Facial puffiness since 15 days.
On 30/4/21 she had a sputum examination which was negative (-) for AFB. On 4/5/21 she was started on empirical ATT. This resulted in generalized weakness. A few days after ATT she started developing pedal edema and facial puffiness. The ATT was stopped 16/5/21 on advice of a pulmonologist.
She has drowsiness since 2 days
She has decreased urine output for the past 2 days.
No history of fever, night sweats, cough.
No history of: palpitations, chest pain, burning micturation.
She has been using an indoor chulha for the past 20 years.
HISTORY OF PAST ILLNESS
She has had similar complaints of shortness of breath on and off for the past 20 years assosiated with occasional cough.
She is a k/c/o Diabetes Mellitus for the past 8 years. Currently under treatment.
She is a c/k/o Hypertension currently under treatment.
PERSONAL HISTORY
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel: Regular
Micturation: Normal
Habits/Addictions: Does not consume alcohol or tobacco.
FAMILY HISTORY
No history of DM,HTN, heart disease or stroke.
DRUG HISTORY
Empirical ATT (Rifampicin:600mg, Isoniazid: 300 mg) started on 4/5/21 and terminated on 16/5/21.
Currently being treated for DM with Tab. Zoryl M1 OD
Currently being treated for HTN with Tab.Telma 40 OD.
SURGICAL HISTORY
Operated for intestinal perforation 20 years ago
Caesarean section 21 years ago.
GENERAL EXAMINATION
Patient was drowsy but arousable
She is moderately built.
VITALS:
Pulse rate: 90 bpm
Respiratory rate: 26/min
BP: 130/80 mmHg
Temperature: Afebrile
GRBS: 104mg%
SPO2: 75% at room air
98% with 6 liters of O2
Pallor: present
Icterus: absent
Clubbing: absent
Cyanosis: absent
Lympadenopathy: absent
Edema of feet: present, upto ankle, pitting type.
SYSTEMIC EXAMINATION
CVS:
- S1 and S2 heard
- Parasternal thrill +
- Diffuse Apex beat felt at 5th ICS
RS:
- Barrel shaped chest
- Bilateral air entry +
- B/l coarse creptes +
- End inspiratory wheeze +
Barrel shaped chest.
ECG:
17/5/21
18/5/21
8:09 AM
6:40 PM
21/5/21
18/5/21:
Na: 125 mEq/L
K: 3.5 mEq/L
Cl: 88 mEq/L
- Total bilirubin: 1.75 mg/dl
- Direct Bilirubin: 0.85 mg/dl
- AST: 94 IU/L
- ALT: 13 IU/L
- ALP: 142 IU/L
- Albumin: 3.25 g/dl
- Urea: 48 mg/dl
- Creatinine: 1.9 mg/dl
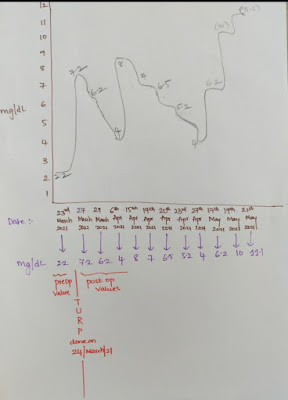
BLOOD PICTURE:
- Hb: 8.1 g/dl
- TLC: 5700
- PCV: 26.8
- MCV: 68.8
- MCHC: 30.2
- Platelets: 2.04 lac
THYROID FUNCTION TESTS:
CXR:
Signet Ring Sign
PROVISIONAL DIAGNOSIS:
Acute exacerbation of COPD associated with right heart failure and bronchiectasis.
TREATMENT:
- Head end elevation
- O2 inhalation to maintain SPO2 above 92%
- Intermittent BiPAP for 2hrs
- Inj. AUGUMENTIN 1.2gm IV BO
- TAB. AZITHROMYCIN 500mg OD
- INJ. LASIX IV BO if SBP greater than 110 mmHg
- TAB PANTOP 40mg PO OD
- INJ. HYDROCORTISONE 100 mg IV
- NEB. with IPRAVENT, BUDECORT 6 hrly
- TAB PULMOCLEAR 100 mg PO OD
- chest physiotherapy
- GRBS 6 hrly
- INJ. HAI SC ( 8 am- 2pm- 8pm)
- Temp, BP, PR, SPO2 monitoring
- I/O charting
- INJ. THIAMINE 1 amp in 100 ml of NS
























































Comments
Post a Comment